Understanding Sacroiliac Joint Stabilization Mechanisms and Movement Rehabilitation: A Comprehensive Guide
- Daehan Kim. M.Sc., NASM-CES, CSEP-CEP., NSCA-CSCS
- Jan 20, 2024
- 8 min read
Introduction:
The sacroiliac joint (SI joint) is crucial in providing stability and support to the lower back and pelvis. It also acts as a shock absorber, distributing forces and minimizing impact on the spine during weight-bearing activities [1]. Understanding the mechanisms involved in SI joint stabilization is essential for those dealing with pain or dysfunction in this area. In this article, we will summarize the anatomy of the SI joint and various mechanisms contributing to its stability.
Anatomy of the SI joint:
The sacroiliac joint is formed by the connection between the sacrum (the triangular bone at the base of the spine) and the iliac bones of the pelvis.
It is a freely-mobile synovial joint and its cavity is filled with lubricating fluid. Its articular surfaces are covered with cartilage that allows for smooth movement.
Its articular surfaces also provide a unique interlocking mechanism due to their irregular shapes.
Many ligaments surrounding the anterior and posterior aspect of the SI joint prevent excessive motion and shearing force.
The joint is richly supplied with blood vessels and nerves, ensuring essential nutrients and facilitating the sense of motion, position, and pain perception.
Muscles like superficial gluteal muscles and deep hip stabilizers directly connect to the sacrum and ilium and can provide dynamic stability to SI joint.
Stabilization Mechanisms: Stability is another term for "precisely controlled" mobility. Various mechanisms work together to achieve it.
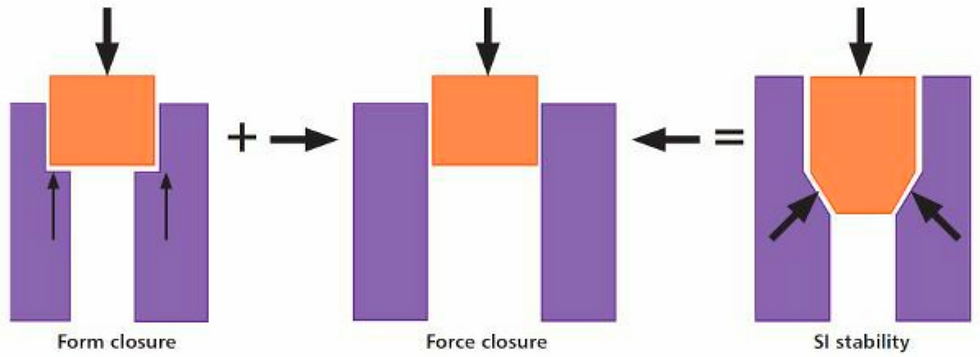
1. Form Closure:
The unique shape and contour of the joint surfaces contribute to the interlocking of the SI joint, minimizing the motion between the two joint surfaces. This is known as "form closure." [2]
2. Force Closure:
"Force closure" adds stability by compressing the SI joint via taut ligaments, muscular force, and tension of other connective tissues like fascia. The force closure facilitates dynamic stability and movement as well as proper alignment during weight-bearing activities. The force closure is especially important for controlling the shearing force when the body weight is supported by one leg as in walking or running [3].
Force closure also reinforces the form closure by increasing the friction between the joint surfaces [1].
3. "Motor control" is fundamental to coordinating force closure and form closure effectively [1]. In this context, "motor control" means the ability to appropriately coordinate muscle activation timing, sequence, and force based on required motion, physical demands to the body, posture, and sensory feedback. Optimizing motor control is the key to successful rehabilitation and is summarized below.
The core muscles, also known as intrinsic stabilizers of the pelvis and spine, proactively generate compression to the SI joint to prepare the body for the upcoming physical demand [4, 5]. For example, when you catch a ball, good motor control will automatically apply an appropriate amount of compression to the SI joint via core activation before the ball lands on your hand.
Proactive compression of the SI joint via core activation is inevitably connected to our breathing because the muscles involved in this mechanism include important muscles for respiration such as the thoracic diaphragm and abdominal muscles. The thoracic diaphragm, abdominal muscles, lumbar multifidi (local stabilizers of the spine segments), and pelvic floor muscles coordinate to generate pressure within the abdominal cavity, called intra-abdominal pressure. This pressure meets the opposing tension from the muscles and connective tissues surrounding the pelvis and lower back [6]. As shown in the picture below, these opposing forces "buttress" the SI joint and lower back. Therefore, SI joint stabilization via core control is more than simply "tightening" the muscles. It is via a fascinating and delicate balance between the intra-abdominal pressure and soft-tissue tension that supports "optimal" (not too much or too little) compression to the SI joint to prepare the body for the impending load.

Importantly, the proactive mechanism explained above also provides preparatory tension to the network of whole-body connective tissues, also known as "fascia". This preparatory tension within the connective tissues is crucial for the adaptive stabilization of the SI joint during limb movement and postural control [7]. Whereas the proactive compression of the SI joint is highlighted by the buttressing force from all 360-degree angles, the adaptive stabilization of the SI joint during movement and dynamic postural control is characterized by selective and direction-specific tension. For example, when our front foot lands on the ground while walking, the body must be able to properly load the body weight onto that foot while preparing to progress the pelvis and upper body forward. Since this occurs with the legs in a split stance position, an additional force to stabilize the SI joint in a diagonal direction is required to prevent excessive shearing while allowing the required motion between the joint surfaces [8]. In healthy individuals, such diagonal stability is almost automatically provided by the muscular action that stabilizes the lower body and the opposite side of the spine and the head, thereby diagonally tensioning the ligaments of the SI joint [9]. This ligamentous tension via the upper and lower body muscle actions is generated because these muscles are essentially connected through the fascia [7]. The image below describes such a connection.
The groupings of muscles and fascial networks that provide selective dynamic stability to SI joints are known as "myofascial slings" [9]. These "myofascial slings" are also important for adaptive change of the direction-specific forces that stabilize the SI joint. For example, as we continue to step forward for walking or running, the pelvis and upper body rotate gradually, which also requires the diagonal stabilizing force to gradually change its orientation. Again, in healthy individuals, such adaptive change of the stabilizing force occurs almost automatically as the myofascial slings that are activated via the natural swinging of the arms and trunk rotation modulate the direction of the forces acting on the SI joint [9]. An example of this myofascial sling is demonstrated in the picture below.
It is important to note that the proactive control of intra-abdominal pressure via core muscles prepares the effective tensioning of the "myofascial slings" as it takes off the slack and gently stiffens the fascial tissues ahead of time. This mechanism is also known as the "hydraulic amplifier" effect of the core [10]. It is a beautiful mechanism that catches two birds at the same time: A) it provides segmental stability of the spine and pelvis, and B) it prepares the whole-body myofascial slings by taking off the slack within the connective tissues and fascia [9]. The image below can help with visualizing this mechanism.
Sensory-motor coordination is another fundamental aspect of motor control that facilitates smooth cooperation between the core muscles and the myofascial slings for SI stability. Sensory-motor coordination refers to the ability to generate the optimal combination of muscle forces and joint actions in a situation-specific manner by integrating multi-sensory information. The multi-sensory integration informs the nervous system about the external environment, the current state of the body, and anticipated forces and stimuli that will act on the body's system so that appropriate and timely motor control can be made [11]. For example, myofascial slings that are typically used for one-leg stability in walking are much more proactively engaged before the foot strikes the ground in running [12]. This is because the nervous system anticipates much greater ground reaction forces at foot-strike in running than walking. This means that the anticipatory core activation and whole-body myofascial control of SI stability are not truly separate mechanisms. They are rather blended in a context-specific way for optimal stability and function thanks to sensory-motor coordination. Once the foot is on the ground, fine-tuning of the muscle activation occurs, adapting to the changing magnitude and orientation of the ground reaction force. The need for this fine-tuning is rapidly signaled throughout the whole body via the tensional change of the myofascial system as the muscles and connective tissues are richly supplied with the sensory receptors to detect the tension change [13].
Every force acting on the body can challenge the SI stability and must be dealt with promptly [8]. We can imagine that the ground reaction force mentioned above can change in numerous different patterns depending on the shapes and conditions of the ground and the things that we may carry in our hands. In addition, the patterns of change will vary even more depending on the movement we make (i.e., walking, running, jumping, side-stepping, standing from sitting, standing from lying down, etc.). And of course, this becomes incredibly more complex when playing sports. Therefore, adaptability of sensory-motor coordination is the key to maintaining the optimal health of the SI joint in real-life situations. The acuity of sensory perception is fundamental to the adaptability of sensory-motor coordination. Notably, the sensory receptors in the myofascial network respond differently depending on specific loading patterns and specific planes of motion [13]. This means that variable movement training is important for developing the sensory acuity for SI stability. In addition, experiencing different patterns of sensory feedback through various movements is important for our nervous system to develop its ability to predict and prepare for timely fine-tuning of muscle activation [14]. For this reason, whole-body movement training in various positions and with variable loading should be integrated into SI rehabilitation training.
Summary of key points
The sacroiliac (SI) joint is crucial for transferring forces between the upper and lower body and absorbing the impact forces into the body.
The optimal balance between stability and mobility of the SI joint is achieved structurally through form closure and functionally through motor control of the myofascial network.
The adaptability of sensory-motor coordination is essential for maintaining optimal SI joint health in various real-life situations.
Specific core training and varied movement training should be integrated for effective SI rehabilitation.
References
Vleeming, A., & Schuenke, M. (2019). Form and force closure of the sacroiliac joints. PM&R, 11, S24-S31.
Forst, S. L., Wheeler, M., Fortin, J. D., & Vilensky, J. A. (2006). The sacroiliac joint: anatomy, physiology and clinical significance. Pain physician, 9(1), 61.
Vleeming, A., Stoeckart, R., Volkers, A. C. W., & Snijders, C. J. (1990). Relation between form and function in the sacroiliac joint: Part I: Clinical anatomical aspects. Spine, 15(2), 130-132.
Kolář, P., Šulc, J., Kynčl, M., Šanda, J., Čakrt, O., Andel, R., ... & Kobesová, A. (2012). Postural function of the diaphragm in persons with and without chronic low back pain. journal of orthopaedic & sports physical therapy, 42(4), 352-362.
Hodges, P. W., Butler, J. E., McKenzie, D. K., & Gandevia, S. C. (1997). Contraction of the human diaphragm during rapid postural adjustments. The Journal of physiology, 505(Pt 2), 539.
El Bojairami, I., & Driscoll, M. (2022). Coordination between trunk muscles, thoracolumbar fascia, and intra-abdominal pressure toward static spine stability. Spine, 47(9), E423-E431.
Willard, F. H., Vleeming, A., Schuenke, M. D., Danneels, L., & Schleip, R. (2012). The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of anatomy, 221(6), 507-536.
Pool-Goudzwaard, A. L., Vleeming, A., Stoeckart, R., Snijders, C. J., & Mens, J. M. (1998). Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to ‘a-specific’low back pain. Manual therapy, 3(1), 12-20.
Gibbons, J. (2017). Functional anatomy of the pelvis and the sacroiliac joint: A practical guide. North Atlantic Books.
Norris, C. M. (1995). Spinal stabilisation. Physiotherapy, 81(2), 64-72.
Johansson, R. S., & Cole, K. J. (1992). Sensory-motor coordination during grasping and manipulative actions. Current opinion in neurobiology, 2(6), 815-823.
Cappellini, G., Ivanenko, Y. P., Poppele, R. E., & Lacquaniti, F. (2006). Motor patterns in human walking and running. Journal of neurophysiology, 95(6), 3426-3437.
Langevin, H. M. (2021). Fascia mobility, proprioception, and myofascial pain. Life, 11(7), 668.
Kimpara, H., Mbanisi, K. C., Li, Z., Troy, K. L., Prokhorov, D., & Gennert, M. A. (2021). Force anticipation and its potential implications on feedforward and feedback human motor control. Human Factors, 63(4), 647-662.
Image sources
Gibbons, J. (2017). Functional anatomy of the pelvis and the sacroiliac joint: A practical guide. North Atlantic Books.
Netter, F. H. (2010). Netter's atlas of human anatomy. Saunders Elsevier.
https://www.dailybandha.com/2012/08/lengthening-torso-in-forward-bends.html












Very detailed and informative!